What is Diabetes?
Diabetes is a chronic metabolic condition that affects millions of people worldwide. This condition causes problems with the body’s ability to regulate blood sugar or glucose, which can lead to serious complications if not treated properly. Diabetes mellitus, also known as diabetes, is a group of metabolic disorders that results in continually increased blood sugar levels. This happens because either the pancreas does not produce enough insulin or the body’s cells do not respond effectively to the insulin produced.

In this article, we’ll go deeper into the complexities of diabetes, looking at its different types, symptoms, diagnosis, management strategies, and the critical role of lifestyle in reducing its impact.
Types of Diabetes?

Type 1 Diabetes:
Type 1 diabetes is a chronic autoimmune disorder that impacts individuals, often manifesting in childhood or adolescence. The body’s immune system, designed to protect against harmful invaders like viruses and bacteria, mistakenly identifies the insulin-producing beta cells in the pancreas as threats and launches an attack. This relentless assault leads to a significant reduction or complete destruction of these crucial cells, impairing the pancreas’s ability to produce insulin.
Symptoms of type 1 diabetes:
- Frequent urination
- Increased thirst
- Fatigue
- Extreme hunger
- Unexplained weight loss
- Blurry vision
- Slow-healing sores
How is type 1 diabetes diagnosed?
Type 1 diabetes is diagnosed through a series of blood tests that measure blood sugar levels and other related signs. Among the most important tests are:
- Fasting Blood Sugar Test: Determines blood sugar levels after fasting overnight.
- Postprandial Blood Sugar Test: Determines blood sugar levels following meals.
- A1C Test: This test measures average blood sugar levels over the previous 2-3 months.
A healthcare professional can also perform tests such as the glucose tolerance test to evaluate the body’s ability to process glucose effectively.
How is type 1 diabetes managed?
Type 1 diabetes is a long-term illness that must be carefully managed throughout one’s life. Insulin therapy is the primary treatment for type 1 diabetes. Insulin injections or the use of an insulin pump are required for people with type 1 diabetes to replace the insulin that their bodies no longer produce. In addition to insulin therapy, people with type 1 diabetes must maintain a healthy diet, exercise regularly, and have their blood sugar levels checked on a regular basis.

Type 2 Diabetes:
Type 2 diabetes is a chronic disease that decreases the body’s ability to regulate blood sugar or glucose. Unlike Type 1 diabetes, which typically manifests in childhood and requires lifelong insulin therapy, Type 2 diabetes is frequently caused by lifestyle factors and can be managed with a combination of lifestyle changes, medications, and, in some cases, insulin. The body either does not produce enough insulin or the cells do not respond properly to insulin in type 2 diabetes. This causes elevated blood sugar levels, which, if not managed properly, can damage various organs over time.
Who Develops Type 2 Diabetes?
Type 2 diabetes is the most common type, accounting for more than 90% of all cases. It is frequently associated with lifestyle factors such as:
- Obesity or excess weight: Approximately 80% of people with type 2 diabetes are overweight or obese.
- Lack of physical activity: A lack of regular physical activity increases the risk of developing type 2 diabetes.
- Diabetes in the family: People who have a family history of diabetes are more likely to develop the disease themselves.
- Age: The risk of developing type 2 diabetes rises with age.
Symptoms of type 2 diabetes:
In the early stages, type 2 diabetes may not cause any noticeable symptoms. However, as the condition progresses, symptoms may include:
- Increased thirst
- Frequent urination
- Extreme hunger
- Unexplained weight loss
- Fatigue
- Slow-healing sores
- Blurred vision
How is type 2 diabetes diagnosed?
- Fasting blood sugar tests and oral glucose tolerance tests help diagnose Type 2 diabetes.
- An A1C test indicates average blood sugar levels over the past 2-3 months.
How is type 2 diabetes managed?
Type 2 can be controlled with a combination of lifestyle changes, medication, and regular monitoring. Among the lifestyle modifications are:
- Diet: Maintaining blood sugar levels requires a healthy diet rich in whole grains, fruits, vegetables, and lean protein. Reducing your intake of processed foods, sugary drinks, and unhealthy fats can also help.
- Exercise: Getting 30 minutes of moderate-intensity exercise on most days of the week can help improve blood sugar control and overall health.
- Weight management: Maintaining a healthy weight can help in the reduction of insulin resistance and the improvement of blood sugar control.
- Stress management: Symptoms can be worsened by chronic stress, making blood sugar control more difficult. It can be beneficial to find healthy ways to manage stress, such as yoga, meditation, or spending time in nature.
- Regular sleep: Adequate sleep is essential for overall health and diabetes management. Each night, aim for 7-8 hours of quality sleep.
- Quitting smoking: Smoking is a significant risk factor for diabetes complications. Quitting smoking lowers the risk of developing these complications significantly.
Medications to help manage blood sugar levels may also be prescribed. The type of medication will be determined by the individual’s needs and response to lifestyle changes.

Gestational Diabetes:
This type of diabetes occurs only during pregnancy. Pregnancy hormone changes can cause insulin resistance, resulting in high blood sugar levels. Gestational diabetes usually resolves after childbirth, but women who have had gestational diabetes are more likely to develop type 2 later in life.
How is Gestational diabetes diagnosed?
Gestational diabetes is usually diagnosed between the 24th and 28th weeks of pregnancy. A blood test called a glucose tolerance test (GTT) is used to diagnose gestational diabetes. The GTT measures blood sugar levels after drinking a sugary solution.
How is Gestational diabetes managed?
- A diet high in whole grains, fruits and vegetables, lean proteins, and low-fat dairy products is advised.
- Limiting carbohydrate intake helps in blood sugar management.
- Eating at regular intervals helps to keep blood sugar levels stable.
- Regular, moderate exercise, such as walking, is beneficial. Obtaining approval and guidance from healthcare providers regarding exercise routines is critical.
- Regular monitoring, often done several times per day, helps track blood sugar levels and ensures that treatment plans are adjusted as needed.
- In some cases, medication or insulin therapy may be prescribed to help manage blood sugar levels effectively.
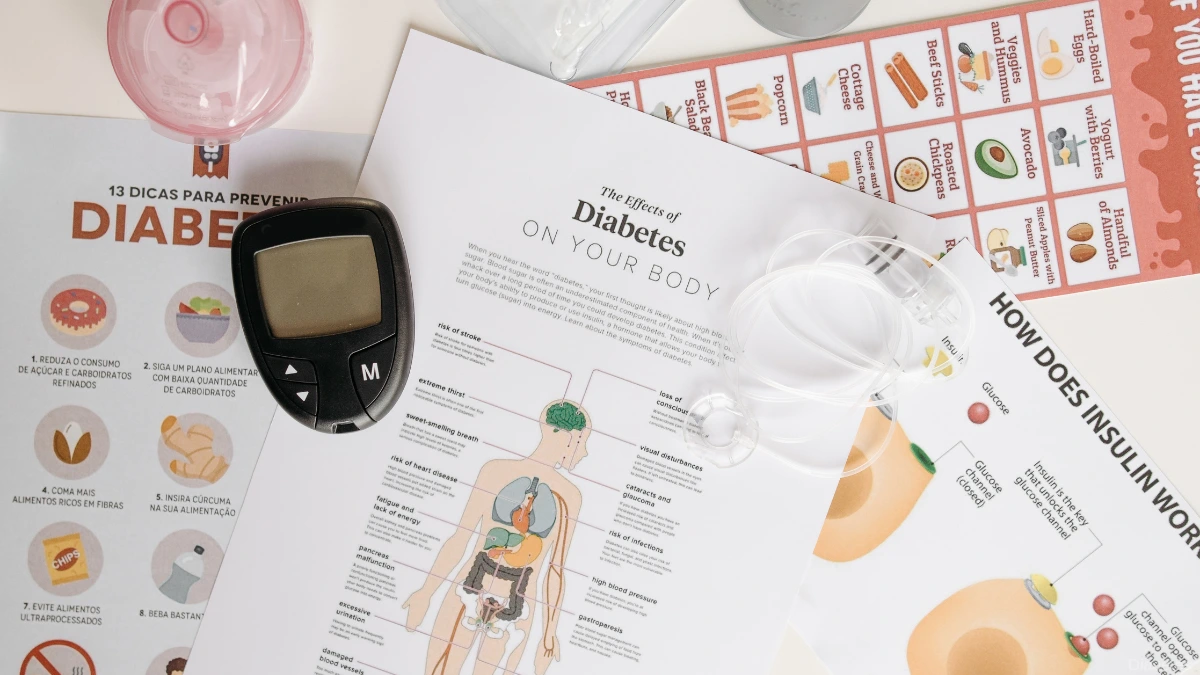
Complications of Diabetes:
Short-term Complications:
1. Hypoglycemia: Low blood sugar levels can lead to dizziness, confusion, and, if severe, unconsciousness.
2. Hyperglycemia: High blood sugar levels contribute to fatigue, increased thirst, and blurred vision.
Long-term Complications:
1. Cardiovascular Issues: Diabetes increases the risk of heart disease and stroke.
2. Nerve Damage (Neuropathy): Numbness, tingling, and pain in extremities due to nerve damage.
3. Kidney Disease: Diabetes is a leading cause of kidney failure.
4. Eye Complications: Increased risk of blindness due to conditions like diabetic retinopathy.

Prevention and Risk Reduction:
1. Balanced Diet: Emphasizes whole grains, lean proteins, fruits, and vegetables.
2. Regular Exercise: Aids in weight management and improves insulin sensitivity.
3. Regular Check-ups and Monitoring: Early detection and intervention reduce the risk of complications.
4. Carbohydrate Management: Consistent carbohydrate intake helps regulate blood sugar levels.
5. Protein and Fiber Intake: Proteins aid in satiety, while fiber supports digestive health.
6. Avoiding Sugary Beverages: High sugar content in beverages contributes to blood.
Diabetes is a complex disease that requires ongoing management and lifestyle changes. Individuals with proper care and attention, can live long, healthy, and fulfilling lives. Early detection, regular monitoring, and a commitment to lifestyle changes are all necessary for effective diabetes management and the prevention of complications.